The menopause journey is unique for every woman. The frequency, duration, and intensity of menopause symptoms can vary dramatically. And, for a small subset of women, the experience is really a non-event. The transition can last up to 10 years (or more), so preparing for each stage can help you manage the symptoms that come with this natural stage of life.
What are the 3 stages of menopause?
- Perimenopause
- Menopause
- Post-menopause
When does perimenopause start?
Perimenopause lasts about 7.5 years on average,
Perimenopause symptoms
“I didn’t realize what was going on. But, that’s when I started with weight gain, and I started a change in menses. It went from regular to being weird, lasting much longer. It was almost like being a teenager again. Didn’t know when it was coming or how long it would last.”
- depression (more likely if you had it earlier in life)
- change in metabolism, weight gain, weight distribution around your waist
- loss of libido
- thinning hair
- generalized aches and pains
- hot flashes and night sweats
- loss of breast fullness
- breast symptoms
- changes in menses – longer/shorter, heavier/lighter, or a combination of these
- worsening of premenstrual syndrome
- headaches
Less common symptoms include new/different body order, gas/bloating/constipation, burning tongue/metallic taste, cold flashes, dry mouth/cavities/loose teeth, and dry eyes.
Studies have shown the likelihood of symptoms may vary depending on your race/ethnicity. For example:
- Hispanic women/Latinas tend to have higher severity scores for constipation, weight gain, and bloating and are more likely to have genitourinary syndrome.
- Japanese women have been noted to have a greater decline in sexual function.
- Indigenous women are reported to have the worst overall menopause experience.
- Black women tend to have more severe VSMs.
“I’ve been kind of tearful, almost like a guilt response maybe, or you feel responsible, you feel guilty. Just a kind of doom and gloom kind of thing. Noticeable to the point that my family and spouse can tell my period is coming. I’m boohooing. I’ve become very sensitive, is another way to put it.”
“I’m not available to my family and kids as much. It’s a two-to-three-day thing. It’s kind of better than worse. It fluctuates.”
“It’s difficult at home and at work, sometimes talking in front of committees and hospital boards. I can’t really afford to be an emotional mess in front of people. So, it affects me in that way. It’s hard to schedule when you’re doing something around your period and your emotional response.”
Throughout perimenopause, symptoms may change or evolve.
Hot flashes, night sweats, and sleep disturbances may start to improve.
Other symptoms like genitourinary syndrome (GSM) – a constellation of symptoms that includes vaginal dryness, painful penetrative sex, frequent UTIs, needing to get to the bathroom quickly to urinate (urgency), needing to urinate more often (frequency) – may appear or become more predominant.
And remember, you can still get pregnant if you have an intact uterus and ovaries and are not infertile.
The Menopause Society discussed perimenopause symptoms with Dr. Monica Christmas, discussing the most common and distressing symptoms, changes to your menstrual cycle, vasomotor symptoms, and mood swings.
Preparing for perimenopause
Be ready to ask questions and persist until you get answers, which may mean learning to be more assertive and moving out of your comfort zone.
“I had to take control of it. I think my gynecologist felt so bad when I was sobbing in her office,” she said. “My primary has been, I would say, the most beneficial healthcare provider in my life because she understands I’m not crazy…She takes matters into her own hands as well.”

What is menopause?
What age does menopause start?
Factors that increase the likelihood of later onset than average include being overweight/obese, having a later age pregnancy/multiple pregnancies, having your first period at age 13 or older, eating habits (diet high in fruit, vegetables, oily fish, legumes, zinc, B6, high total calories), moderate alcohol consumption, and Japanese ancestry.
Join the community!
LEARN • SHARE • LAUGH • BOND
The menopause journey community is a private online community powered by pausitive health. It’s a safe space for women+ to connect, learn, share, laugh, and bond through their menopause journey.
It’s free to join! We hope to see you there.
Menopause symptoms
“…it’s not just hot flashes. And I didn’t know that. It’s the sleep disturbances. When I lie awake in bed, I just have awful heart palpitations. The pulsating I even have up to my jaws. The most bizarre things.
So, I did some research and see heart palpitations is something that seems related to menopause.
There are days you just feel so crazy and so out of control. And you can see yourself and feel yourself being a little nasty or whatever, and you just can’t help yourself. That’s just a hormone thing.”
Another survey participant who experienced menopause in her early 40s said memory loss troubled her most.
“The mental fogginess was terrible, and it’s only gotten a little better after I‘ve completed menopause,” she said.“…. I would go to my office and cry. Just thinking about it now brings some tears. Because I pride myself on knowing what I’m doing and doing a good job, and suddenly my brain just didn’t work like it used to. And I was going back to grad school at the time. It was terrible. It was awful,” she recalls.
“If I could go back and tell myself, ‘look, you have to write this stuff down because you’re going to forget it,’ it would still be upsetting, but I think I wouldn’t have those embarrassing moments in the classroom.”

Post-menopause symptoms
In the women we surveyed, respondents described their post-menopause journey as eventful to life-altering.
For one, it was liberating.
“You don’t have to worry about having periods, don’t have to worry about having tampons, don’t have to worry about pregnancy, and that’s a huge freedom.”
Knowing she’s at this point, she looks back, reflects, and uses what she experienced on her journey to help three of her colleagues going through their own menopause journeys.
“I tell them, watch out for the brain changes. I wasn’t ready for that, and I’m telling you, you’re not stupid,” she said.
Showing empathy toward others can help you more than you imagine.
What signals the end of menopause?
So, once you’re past menopause and in the post-menopause stage, how soon until it all ends? Technically, never!
The post-menopause stage of the journey is the rest of your life. You may experience fewer symptoms. However, they may not disappear completely and can stick around for years.
The Penn Ovarian Aging Study cohort assessed women for 16 years. On average, women experienced moderate to severe hot flashes for nearly five years after menopause. The study found hot flashes did not return to premenopausal levels until nine years after the woman’s final menstrual cycle.
And a Mayo Clinic study of 5000 women found some women in their 60s, 70s, and 80s continued to experience menopausal symptoms. Caffeine consumption appeared to increase the likelihood of symptoms in those older than 70.
Treatment options throughout the life cycle of menopause

Prepare yourself and embrace the menopause journey
If you haven’t dialed in on a healthy lifestyle, now is the time to do it. Get a menopause roadmap to prepare for the menopause marathon and feel your best.
A life-affirming mindset and lifestyle factors are powerful ways to improve your health and well-being.
Take these healthy lifestyle steps early:
- Eat a well-balanced diet, and avoid saturated fat, preservatives, processed foods, sugary beverages, and grilled/charred foods. Try these foods for menopause.
- Engage in physical activity regularly for at least 150 minutes a week with a regimen that includes cardio, weight-bearing, strength training, and flexibility and balance. Try these exercises.
- Avoid being sedentary for extended periods.
- Maintain a healthy weight.
- Limit or eliminate alcohol.
- Get enough sleep of good quality (7 – 9 hours). If you’re struggling, try this sleep hygiene routine.
- Learn techniques to manage stress and build resilience.
- Stop the use of tobacco products.
- Engage in mentally stimulating activities.
- Nurture your relationships.
The pausitive health menopause grocery list contains a combination of foods specifically selected to help you feel better today and even better in the future.
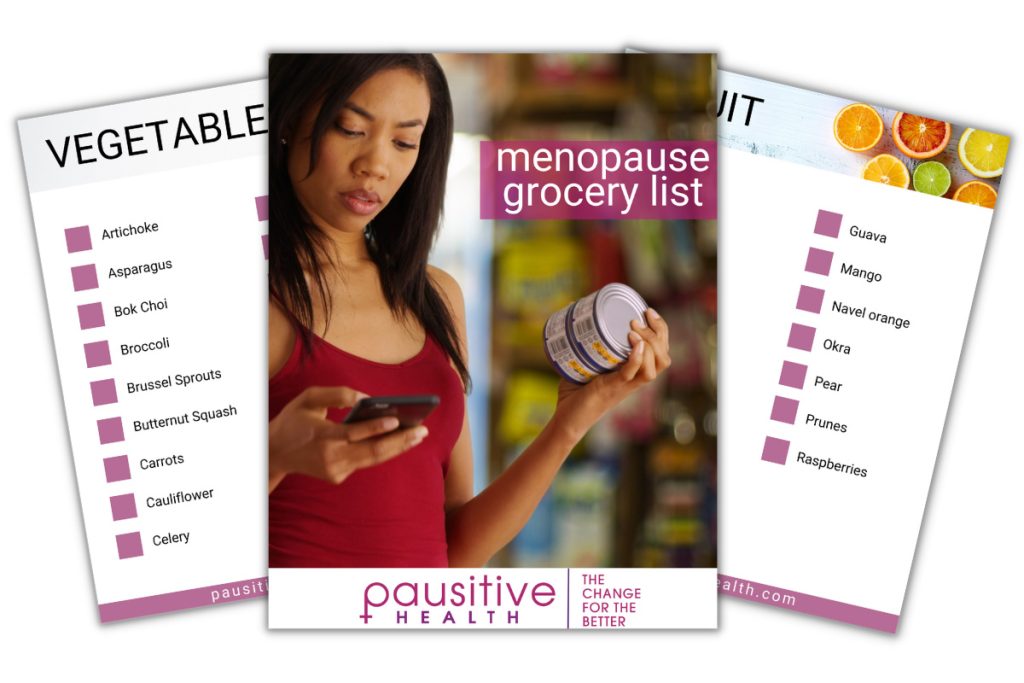
Make A Change For The Better!
This menopause grocery list contains a combination of foods specifically selected to help you feel better today and even better in the future.
Talking to your doctor
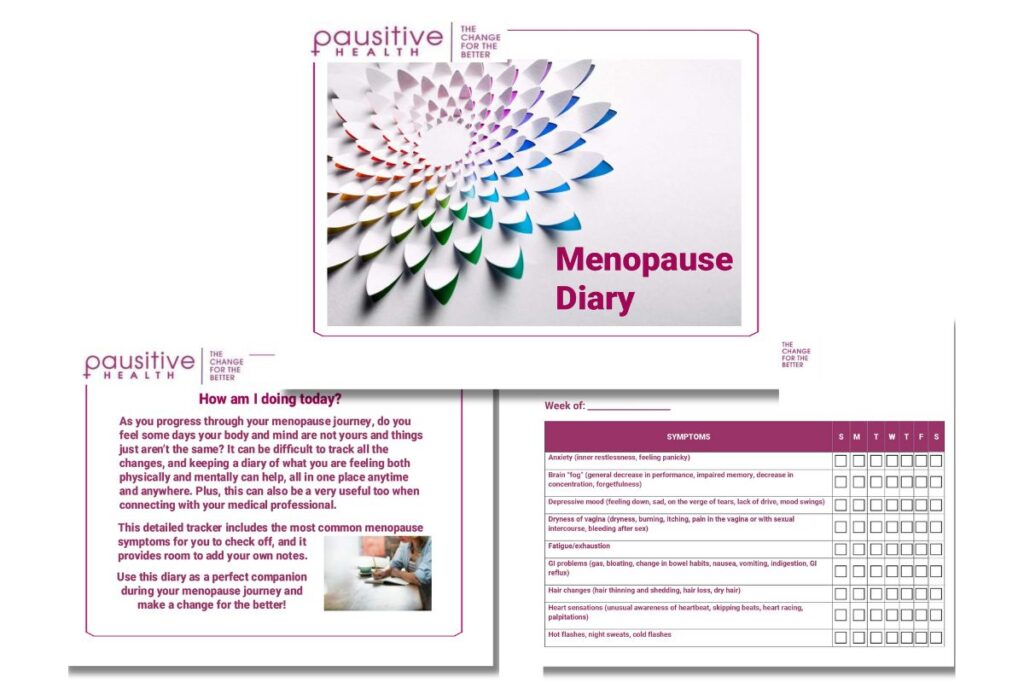
Menopause Diary
How are you doing today? Better than yesterday, or are you experiencing more symptoms? Make it easy to track your symptoms with the Menopause Diary.
While the focus of menopause is often on unwelcome symptoms, think about how you can positively impact your future.
Your mindset can play a major role with regard to your experience. A study performed by Yale found:
- Menopausal symptoms were less of an issue in countries where older women are more highly regarded in general.
- In countries where a phrase like “old age” was viewed negatively and was attached to the menopause stage of the life cycle of women (like the U.S.), symptoms were often more pronounced.
Although it might sometimes be challenging, you can make menopause a positive journey to vibrant living!
Investigating Health for Mid-Life and Older Women | SWAN
Primary ovarian insufficiency | Mayo Clinic
Perimenopause: Signs, Symptoms, and Solutions | The Menopause Society [YouTube]
Find a Menopause Practitioner | The Menopause Society
Eleni Armeni, Nicoletta Mili, Elina Siliogka, Dimitrios G. Goulis, Irene Lambrinoudaki. Menopause medical education around the world: The way forward to serve women’s health. Current Opinion in Endocrine and Metabolic Research. 2022, Vol 26, pages 100387. https://doi.org/10.1016/j.coemr.2022.100387
Kling J, MacLaughlin K, Schnatz P, Mara K, Fohmader Hilsaca K, Faubion S. Menopause Management Knowledge in Postgraduate Family Medicine, Internal Medicine, and Obstetrics and Gynecology Residents: A Cross-Sectional Survey. Mayo Clinic Proceedings. 2019. Volume 94, Issue 2, P242-253. doi: https://doi.org/10.1016/j.mayocp.2018.08.033
Be a Healthcare Rebel: How to Get the Best Medical Care | PeopleTweaker
What is Menopause | National Institute on Aging
25 years of research shows insidious effect of racism on Black women’s menopausal transition, health | University of Michigan
Alejandra Andrea Roman Lay, Carla Ferreira do Nascimento, Bernardo Lessa Horta, Alexandre Dias Porto Chiavegatto Filho. Reproductive factors and age at natural menopause: A systematic review and meta-analysis. Maturitas. 2020. Volume 131, P57-65. DOI:https://doi.org/10.1016/j.maturitas.2019.10.012
Menopause: Mindfulness may reduce symptoms | Healthline Media
About Guided Imagery | Images of Wellness
News flash about hot flashes: They can last longer than you think | Science Daily
Culture may influence how women experience menopause | Reuters
Freeman EW, Sammel MD, Sanders RJ. Risk of long-term hot flashes after natural menopause: evidence from the Penn Ovarian Aging Study cohort. Menopause. 2014 Sep;21(9):924-32. doi: 10.1097/GME.0000000000000196. PMID: 24473530; PMCID: PMC4574289.
Vaze N, Joshi S. Yoga and menopausal transition. J Midlife Health. 2010 Jul;1(2):56-8. doi: 10.4103/0976-7800.76212. PMID: 21716773; PMCID: PMC3122509.
You may also like…

Why Your Doctor Might Not Be Well-Informed About Menopause And How To Take Action
Has your doctor asked you menopause? Learn why your doctor may not be well-informed and how you can find a menopause doctor.

Foods For Menopause: 9 Best Foods To Help Menopause
Did you know you can manage your menopause symptoms with food? Learn the 10 best foods packed with the necessary nutrients to feel better.

Prepare for Menopause Like A Marathon: Your Body Will Thank You
Menopause is a marathon, not a sprint. You have the opportunity to enhance your health and well-being for the rest of your life. And, just like the 26-mile run, preparation for the “Menopause Marathon” is key to reaching the finish line. Focus on your body, mind, and spirit so you can feel your best during this natural stage of life.